2020/21 was an extremely challenging year for the Men’s Health Forum, but our work has never been so important.
The COVID-19 pandemic has thrown the challenges of men’s health into stark relief:
- Men have been 63% of premature UK deaths from COVID
- Men’s health inequalities are laid bare by COVID – with, for example, men from the ‘Black Caribbean’ ethnic minority group being 2.7 times, and men from the Bangladeshi group being 3.0 times more likely to die from COVID than men from the ‘White British’ group during the first wave of the pandemic in England and Wales – and similar differences comparing areas with different areas of deprivation
- Sex and gender have played and continue to play a significant role in compliance with and attitudes towards government guidelines on preventative behaviours such as lockdown, mask-wearing and social distancing
- The historically poor engagement of the health system with men has been reflected in the vaccination programme with lower vaccination rates among men in every age group, especially younger men
Our work to raise awareness and drive policy change was our top priority across the year
- Maintaining and extending an entire new COVID section of our website – with up-to-date statistics, insight, analysis and men’s perspective on COVID
- Running Men’s Health Week 2020 virtually – with a well-attended webinar on Men & COVID with Professor Gurch Randhawa, Professor Alan White and Peter Baker – highlighting the challenges faced by BAME men, an online Toolbox Talk training session – and running our first “Men’s Health Chat” via Zoom
- Creating – and updating – new materials for the workplace, including a new Toolbox Talk and a COVID-focused Man Manual.
- Making submissions to the Women & Equalities Committee in the UK Parliament, to ministers, parliamentarians and to the NHS and Public Health to highlight the specific challenges faced by men
- Being one of the first to highlight the risk on men and COVID vaccination across England, Wales and Scotland – and successfully persuading the UK JCVI to strongly highlight the COVID inequalities faced by men and instruct the health system to take action on them.
At the same time, COVID forced major changes on how we work – and required us to innovate and change how we generate and use our funds.
Winning policy change
One the biggest frustrations and challenges of the year has been getting the Government and health system to respond adequately to the higher health impacts of COVID amongst men.
As soon as the vaccine was announced, we wanted to understand what sex and gender impacts there were likely to be - setting up an online survey to gain insight into men’s attitudes to vaccination and recruiting men for more in-depth interviewing, reaching out to academic partners to ensure we were looking at the latest relevant research, alongside reviewing the significant amount of published data on men’s attitudes to the issue.
This preparatory work enabled us to provide a very fast turnaround to a ministerial request for information that came out shortly before Christmas 2020 via the Department of Health & Social Care (DHSC) Health & Wellbeing Alliance – highlighting the challenges faced by black and minority ethnic (BAME) men, working-age men and men who think they’ve had COVID.
A particular concern was men’s greater risk was not adequately reflected in early JCVI (Joint Committee on Vaccination & Immunisation) guidance (with some surprisingly poor analysis early on regarding the extra risk faced by men) – and getting this addressed was a top priority.
To this end, we wrote to all committee members of the JCVI setting out our concerns and asking for explicit reference to men’s greater risk in any future guidance.
Gratifyingly, it worked. The revised guidance issued in February 2021 and updated in April 2021 stated:
In individuals aged 18 to 49 years there is an increased risk of hospitalisation in males, those from certain ethnic minority backgrounds, those with a body-mass index (BMI) of 30 or more (obese or morbidly obese), and those experiencing socio-economic deprivation.
JCVI strongly advises that individuals in these groups promptly take up the offer of vaccination when they are offered, and that deployment teams should utilise their understanding of local health systems and demographics, combined with clear communications and outreach activity, to promote vaccination in these groups.
Unvaccinated individuals who are at increased risk of severe outcomes from COVID-19 on account of their occupation, male sex, obesity or ethnic background are likely to be vaccinated most rapidly by an operationally simple vaccine strategy.
The challenge of getting adequate action taken to follow through on this advice remains a high priority, but it is hard to underestimate the importance of having this guidance in place to enable us to do so.
Wider policy challenges
While the response to COVID was our highest policy priority, our work with the DHSC Health & Wellbeing Alliance meant that we continued to work on a wide range of other policy areas:
- We actively contributed to NHS England’s Beneficial Changes work – seeking to identify and embed positive changes that had happened in response to COVID
- We supported PHE’s new F.A.S.T stroke campaign – discussing gender insights on strokes and publicising their new campaign
- We supported National No Smoking Day and highlighted the impact of smoking on mental health and in our COVID materials
- We served on the External Advisory Group of the Sexual & Reproductive Health team at PHE – with a particular interest in their Male Reproductive Health Survey work – and continuing to oppose the proposal to stop asymptomatic screening for chlamydia amongst men
- We sought to ensure that NHS-X properly accounted for gender in their work on digital uptake – highlighting the challenge that men are greater users of digital, but lower users of NHS digital services
- After engaging with the bowel cancer screening team at PHE, we updated our information to reflect the impact of the new FIT test – which is increasing screening uptake amongst men
- We signed the PHE Healthy Ageing Consensus Statement and continued to work with the UK Men’s Sheds Association and sought to ensure that their insights were reflected in PHE’s work
- We continued to engage with the Obesity & Healthy Weight team at PHE to ensure that future investment adequately addressed the under-representation of men in weight management services
- In addition, we worked with other DHSC Health & Wellbeing Alliance partners on a range of other projects including VCSE data & intelligence sharing, reducing parental conflict and health inequalities for older people in rural and coastal areas.
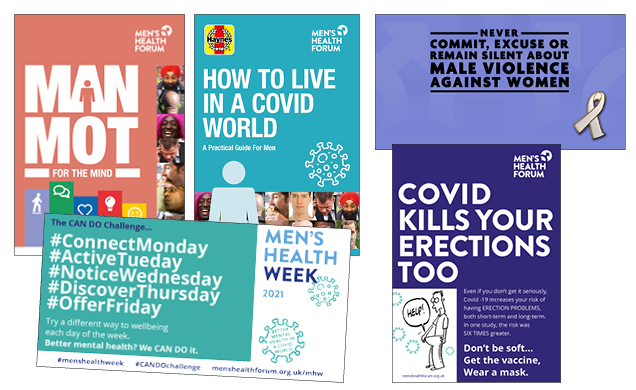
Towards the end of the year, the tragic murder of Sarah Everard brought the issue of male violence to the fore. While the debate around male violence rightly focused on women, it is a huge issue for men’s health as well. We took the opportunity to promote our support for the White Ribbon campaign and highlight our commitment to gender equality.
I promise to never commit, excuse or remain silent about male violence against women.
Continue provision of health information for men
Our primary method of engaging men continued to be our website and we continued to drive our online and offline communication with men in 2020/21 – with 1.4 million visitors to our website, up 6% vs. the previous year, and 2 million page-views, up 10%.
Our men’s health group on HealthUnlocked now has more than 25,000 members and our new penis health group has more than 19,000.
The number of people signed up for our email news grew by 24% to over 7,300. The number of Twitter followers increased to just under 13,000.
Our pace of launching new printed Man Manuals had to slow – since there was less interest in these with so many people working at home: ‘Man MOT for the Mind’ was well received. Though carefully written to avoid going out of date, ‘How to live in a COVID World’ performed disappointingly.
Our shift to digital manuals meant that our content was reaching large numbers via company intranets – with orders from large organisations like Costa, Wates, Tate & Lyle and Hampshire Police – although we have no means of tracking the exact reach of these manuals currently.
Facing our funding challenges
Despite the strong reach of our activities, 2020/21 was very challenging financially, with bulk sales of our Man Manuals dropping by two-thirds – and limited government support for charities working (as we were) out of shared offices.
In response we cut cost sharply, reducing headcount for much of the year (through leaving a post unfilled) and closing our office, with all staff working from home, and a move to virtual Trustee and staff meetings.
We also introduced new ‘digital bespoke’ manuals – suitable for companies that wished to share our information with staff working at home – and launched a very successful new online “Men’s Health Champion” training programme. The time spent putting robust fundraising infrastructure in place – such as direct debits – paid off with a trebling of donations. We particularly appreciated an £8,000 corporate donation from the DPD Group in March 2021.
We owe a huge debt to our staff and associates across the year – Martin Tod, Jim Pollard, Paul Millar, Chris Stein and Peter Baker for making all this change possible and all their work in the face of these challenges.
Our last year in the DHSC Health & Wellbeing Alliance also played a vital role in keeping us going – although the associated workload also went up with much more frequent online meetings and requests for information. Sadly, our long and productive association with the Alliance finished at the end of the year since we did not meet the qualifying criteria to apply for their 2021/22 programme.
Looking to the future
Although the last year has been focused on the immediate challenges of the pandemic, it’s clear that in the future, we must redouble our efforts to secure a men’s health strategy for each of the UK nations. Men’s health was already bad: COVID has made it worse.
The launch of the women’s health strategy consultation in March 2021 presents a tremendous opportunity. The Government has, in effect, conceded the need to better recognise sex and gender in healthcare. We will learn from the approach taken by those who successfully campaigned for a women’s health strategy and build a strong coalition for change.