The year 2021/22 saw the end of pandemic restrictions, continued change to the way we work and the way we get our information to men, strengthened fundraising and the launch of our joint campaign for a Men's Health Strategy.
Ongoing campaigning on Covid
Even as the pandemic receded, sex and gender continued to play a strong role in all aspects of it - outcomes, behaviours and engagement.
While in the early stages, our concern was getting action that reflected the higher mortality rate amongst men, as the vaccination rolled out, it became clear that, despite the expectations of the government and academic attitudinal research, we were starting to see an emerging gender gap in vaccination rates among working age men in England and younger men in Scotland.
After contacting various bodies - and the media - to try and get traction on the male vaccination shortfall, and sharing insight into the attitudinal reasons that needed to be addressed, we reached out to the NHS England Voluntary Sector team - our former contacts for the Health & Wellbeing Alliance - and started working with NHS England to close the vaccination gap amongst working age men - meeting the Head of Vaccines Equality to discuss the shortfall amongst men - and what action could be taken.
We also tried to use our contacts in the global men's health movement to raise awareness - presenting on vaccination rates to the Men & COVID sub-group of the global Gender and Covid-19 Working Group - and quickly turned around a campaign highlighting the link between Covid-19 and erection problems.
Ultimately, Covid-19 was a perfect storm for men's health and an illustration of why we need to keep working for change. Men were 65% of those hospitalised from COVID and 61% more likely to die from COVID. The inequalities between men that we have seen in other areas have been reflected in COVID, with, for example, men in England from the 'Black Caribbean' group 2.6 times more likely to die from COVID as white men in England during the first wave of the pandemic, and 4.2 times as likely to die from COVID as white women in England.
Men's behaviour, compliance and response to government guidelines on testing, mask wearing and social distancing have been different at every stage - and very little visible work was done by government to understand them or respond to them.
Even though we seem to be past the worst of the pandemic, the health system remains consistently less effective in engaging with men - with lower vaccination rates amongst men in every age group, particularly younger men - dramatically lower testing rates amongst men - and a bigger drop in GP attendance during the pandemic for men than for women. The moment has passed for major change - although we continue to try to ensure that the issue of men's health is reflected in ongoing analysis of the pandemic and highlight how the lessons to be learned from the pandemic can be reapplied to men's health.
Our first 'post COVID' Men's Health Week
As we moved towards our first post-pandemic Men's Health Week in June 2021, for the first time in recent memory, we held a pre-Men's Health Week discussion with potential participants, following the example of our Irish colleagues, which led to significant and productive improvements to our plans - especially the introduction of the 5-day 5-ways to wellbeing CAN DO Challenge.
Our original plan focused on men's post-COVID mental health, but feedback from potential partners indicated that they needed positive campaign messages to deploy in the workplace - so we extended the 'CAN DO' challenge and called on everyone to choose a different way to wellbeing to try each day of Men's Health Week. The five ways are (and were):
- Connect - connect with other people (eg. call an old friend you haven't since before lockdown) #connectmonday
- (Be) Active - move your body (eg. go for a run/walk/swim/dance/etc) #activetuesday
- Notice - take notice of the environment around you (eg. turn off your phone for an hour) #noticewednesday
- Discover - learn something new (eg. read a book you haven't read before) #discoverthursday
- Offer (or give) - do something for someone else (eg. volunteer for a local community group) #offerfriday
Alongside this, we also campaigned to raise awareness of post-COVID mental health and to recruit people to sign our Men's Health Strategy petition.
We welcomed partners who joined us in campaigning during the week - partnering on the Shameless Cycle Ride with myGP and with the vocal group the Overtones on social media.
Restoring our finances - stronger fundraising - new types of training & publications
As expected, we faced a sharp drop in revenue in 2020/21 as new eligibility criteria blocked us from bidding for the DHSC Health & Wellbeing Alliance programme that has been an important source of funds for us in the past. This required us to scale back our operations - cutting cost and reducing staff - and confirming the move to virtual working as we moved the contents of our office to a storage unit - and moved our office address to a 'virtual' HQ back in Southwark at the Canopi Borough shared office space.
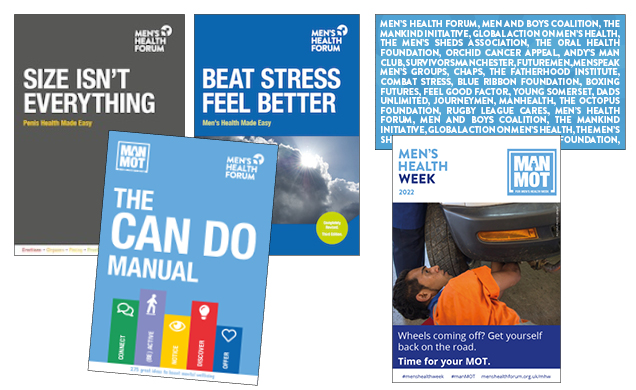
To compensate, we continued to innovate and change our publications and training – with continued strength in our new online 'Men's Health Champion' training, new online publications and a dramatic expansion in bespoke publications, as new printing technologies allowed us to quickly and affordably supply companies that wanted to share men's health information with their employees with high quality printed health manuals - in any size of print-run between 25 and 25,000.
After a concerning slow down as pandemic lockdown ended, our training and publications recovered well. Our website continued to play a vital role with 948,000 visitors and 1,338,000 page views. We now have over 13,000 followers on social media, 9,500 people receiving our regular emails and more than 28,000 people have engaged in our forums on Health Unlocked.
We also continued to develop and launch new content - including Size Isn't Everything - an online PDF publication sponsored by Viatris, a new Stress at Work Action Plan (SWAP), and a refreshed 3rd edition of Beat Stress, Feel Better.
Our continued work to make it easy to donate to us - enabling people to give via Amazon Smile, the Charities Aid Foundation, the PayPal Giving Fund, Facebook, JustGiving and TotalGiving - led to increased revenue. We were particularly grateful for a £14,000 unrestricted grant from the Tudor Foundation and the launch of a year-round fundraising programme by Cllr Greg Rattey as one of his mayoral charities in his first year as Mayor of Sawbridgeworth. Our new edition of Beat Stress, Feel Better was made possible thanks to donations in memory of James Kelly (1978-2022).
Building partnership: campaigning for a Men's Health Strategy
After making progress running our Men's Health Strategy campaign on a standalone basis, we concluded we could accelerate the pace and increase its impact through improved partnership working. We held an inaugural meeting and starting to recruit other organisations in support - including Global Action on Men's Health (GAMH), Mankind Initiative, Men and Boys Coalition, UK Men's Sheds Association and Orchid. This grew over the summer - with recruitment of further partners such as the Patients Association and Prostate Cancer UK - and presentations to the All-Party Parliamentary Group on issues affecting men & boys in July and October - also raising the issue at the Cross-Party Group for Inequalities in Scotland - and culminated in the launch of our case for a men's health strategy on November 17, 2021.
Following the launch, new partners - both corporate and individual - and including leading academics in the world on public health and men's health - continued to back the campaign.
Increasing numbers of people continue to sign-up to back the campaign and access the case for a men's health strategy via menshealthforum.org.uk/strategy
Applying partnership more widely
In addition, we continued to partner with other organisations - including on some work remaining from the DHSC Health & Wellbeing Alliance:
- Joining the launch and backing the dissemination of the DHSC Health & Wellbeing Alliance project: VCSE data & intelligence - looking at how voluntary sector organisations can use data and intelligence to help the health system support their beneficiaries more effectively.
- Supporting the launch of Alder Hey Foreskin website - https://4skin-health.alderhey.nhs.uk/
- Ongoing support for the University of Stirling's Game of Stones men's weight research project - https://www.gameofstonesresearch.com/Public/Public/index.cshtml
- Participation in the University of Oxford's GP-SUS (Access to General Practice: Innovation, Impact and Sustainable Change) Steering Committee - reviewing GP Access Interventions
- Taking part in a round table on men and cancer organised by the European Cancer Organisation.
- Supporting a new Men's Health Group in the Department of Health & Social Care
Responding on wider health issues
While the Men's Health Strategy campaign has been our primary focus, we have also responded to:
- The Women & Equalities Commons Select Committee Follow Up Work on the Mental Health of Men and Boys
- The NHS Equalities Core20Plus5 strategy - asking that they use a gender-lens while tackling inequalities amongst the groups they identify.
- The independent Khan review: making smoking obsolete - highlighting the continuing role of gender in the levels and type of smoking still prevalent in the UK today
- The DHSC 10-year Cancer Plan - drawing attention to the higher rates of most cancers amongst men, the need for specific prevention measures that target men, supporting Prostate Cancer UK's call to work towards a prostate cancer screening programme for men and the need for better data and reporting on cancer and its impacts amongst men.
Even today, too many men are dying too young
Ultimately, the evidence base for a men's health strategy reinforces the case for us to continue our work.
In 2020, 19% of UK male deaths - around one in five - were before the age of 65.
Men are:
- 75% of deaths from suicide - with suicide the biggest cause of male death under 50
- 76% of premature deaths from heart disease
- 43% more likely to die from cancer
- 63% of premature deaths from Covid-19
- 26% more likely to have type 2 diabetes, and 68.5% of diabetic amputations
- 66% of alcohol-related deaths.
In September 2021, the ONS reported the first decline in male life expectancy since the 1980s.
Society pays a huge cost for this - with 676,000 years of life lost every year in the working age male population in England and Wales (16-64), mostly through avoidable premature mortality.
Aside from the emotional and social consequences, this imposes huge costs in health costs, sick pay and welfare benefits and the economic and tax losses of lives unnecessarily cut short.
And it doesn't have to be this way: a sex- and gender-informed approach to healthcare and prevention will produce better results both for men and for women.
There is plenty to do - and we look forward to working with our supporters and partners to help make it happen in 2022/23.