New research in the London Borough of Haringey has identified four key factors in male engagement with preventative health services.
The Men's Social Marketing Segmentation and Insight Project involved interviews and focus groups with both local residents and health professionals. It identified three groups or 'segments' of males: those who were willing to use GP-led preventative services; those who needed more flexible services to engage; and those who needed proactive supportive outreach to become engaged. Examples of flexibility included being open longer hours and at weekends and availability at community centres and other non-GP facilities.
The project found that across all the segments, there was a lack of knowledge as to what preventative services were actually provided by primary care, or to which GPs could refer patients on to. There was also confusion around the term ‘preventative’ - what it actually meant and who the services were designed for.
The second factor was around ‘fear’ and possibly ‘denial’. ‘Fear’ was not solely related to the outcomes - what tests might find - but also the process. These fears were heightened if individuals were attending GP services as GPs were seen as ‘generalists’ who would just refer to a hospital specialist.
Thirdly, men preferred to have physical examinations and tests (such as blood tests), as opposed to simply ‘talking’ about their problems to the health professional.
Fourthly, ethnicity does not appear to be a factor. Although familial patterns, behaviours and cultural norms were seen to be important within families, no evidence was found that some ethnic groups are more or less likely to access preventative services.
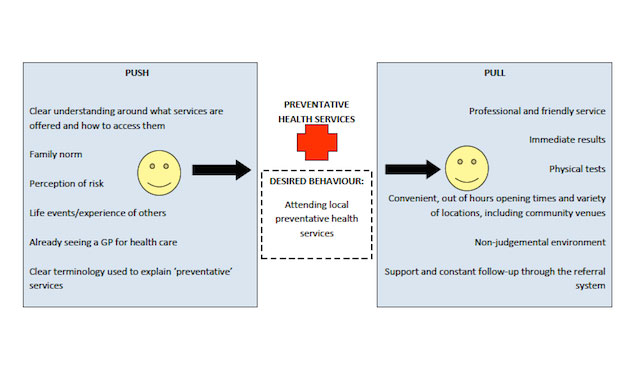
The researchers from the NSMC, formerly the National Social Marketing Centre, identified the pushes and pulls in accessing preventative health servcies (see diagram) and made the following recommendations:
- Conduct basic service improvements to existing clinics, including training for receptionists and health professionals to ensure they have the correct and up-to-date information to give to patients; consistency in offering rapid results; open evenings and weekends; choice of locations (for example, pharmacists and local community centres; physical tests being part of any check; and booking follow-up appointments).
- Address knowledge gaps to ensure that the basic service improvements are made. These include: mapping existing services against the segments; establishing how GP surgeries currently refer people; review past referral systems to understand how they worked; and review the effectiveness (including cost-effectiveness) of the different modules of preventative service delivery.
- Use the segmentation approach to ensure that local services meet the needs of each of the segments.
- Improve stakeholder engagement - the NSMC have found that social marketing projects which have not engaged fully with the stakeholders have been unsuccessful.
Haringey has a strong reputation for tackling health inequalities including those around gender and is a partner in the Men's Health Forum's Haringey Man MOT project.
- The full Men's Social Marketing Segmentation and Insight Project report is available on the Haringey Council website.