MEN'S HEALTH MANIFESTO: Remove the barriers, reach out and make the most of it when men do engage
Remove the barriers to using health care, mental health and preventative care - especially for men of working age:
- Sort out opening times and access so they work for full-time workers
- Improve online access, booking and other interaction
- Stop using drug or alcohol problems as a barrier to mental health treatment – invest in integrated care for dual diagnosis
- Deliver on the recently announced access & waiting time standards for mental health
- Tackle stigma and discrimination, especially in the workplace and especially for men with stigmatised problems such as mental health, eating disorders, breast cancer and sexual violation
- Greater use of self-help groups and peer-led services.
Reach out proactively:
- Take services to where men are: workplaces, online, pubs, sports grounds, betting shops, prisons etc.
- Where it’s not already happening, extend occupational health to include screening and preventative health measures
- Create a ‘Mental Health Diversion Duty’ in the criminal justice system and emergency care – intervening more effectively to reduce the number of people arrested under Section 136. Deliver national coverage by 2017
- Increase health check outreach and uptake amongst men
- Start bowel cancer screening earlier, especially for higher risk men, including MSM.
Make the most of it when men do engage with health services:
- Include cancer symptom awareness, mental health, sleep apnoea and erectile dysfunction in health checks
- Special focus on high-risk infrequent attenders
- Co-design new services with men.
Why is this important?
Health services are still not effectively engaging with men. Especially during working age, men remain less likely to:
- attend a general practitioner
- attend a NHS Health Check
- opt for bowel cancer screening
- visit a pharmacy
- take a Chlamydia test
- have a dental check-up.
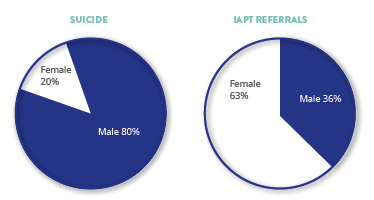
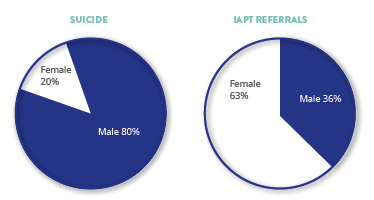
Four in five suicides are male but only a minority of these men were engaged with mental health services.
67% of men are overweight or obese yet only 10-20% of those on NHS weightloss programmes are men.
Research has suggested a link between men’s lower use of primary care and their higher rate of hospital services.
71% of CVD-related deaths under 65 are amongst men14 and the NHS Health Check programme focuses on circulatory conditions, a major killer of men, yet only 35% of local authorities know how many men they reach with the
programme,15 and within those authorities only 44% of health checks are conducted amongst men.
> Next section: Design targeted programmes for the men and boys in greatest need